Preclinical Radiotherapy
The Preclinical Radiotherapy Facility, based at the UCL Cancer Institute, enables multidisciplinary radiation research studies within the CRUK City of London Centre. The Xstrahl SARRP Radiation Research Platform is an image-guided micro-irradiation system, designed for targeted delivery of medium energy x-ray irradiation to experimental models. Research uses include 2D and 3D cell irradiations, targeted tumour irradiations, immuno-radiobiology, and sublethal irradiation.
The irradiator combines a standard 225kV X-ray tube, mounted on a gantry to allow 360-degree rotation around a specimen, with imaging capability for high resolution cone-beam CT imaging. The bespoke Muriplan software enables rapid 3D image acquisition and reconstruction. Target identification, treatment planning and isodose calculations are completed in Muriplan, allowing the dose distribution to be applied similarly to treatment provided during clinical radiotherapy. The radiation field is fully adjustable between 0.5 mm diameter fixed collimator, and 40×80 mm, with a maximum field size of 100 x120 mm at 35 cm source to surface distance.
i) X-ray tube mounted on rotating gantry with collimator attached. ii) Ion chamber dosimetry in solid water. iii) Example CT scan showing tissue definition prior to dose-volume analysis.
Contact
Academic Lead
Equipment
The Xstrahl Preclinical Radiation Research Platform (SARRP) combines CT imaging capability with adaptive radiation delivery. The irradiator consists of an X-ray tube mounted on a 360-degree rotating gantry with a fully adjustable platform, or 3D-printed treatment couch, enabling optimal targeted radiation delivery. A copper filter for treatment and aluminium filter for imaging are fitted for beam refinement. A CT detector panel is positioned facing the X-ray tube for use when cone-beam CT imaging is required.
Beam collimators restrict the path of the X-ray, narrowing the beam for radiation targeting. Interchangeable fixed brass collimators of 0.5 mm to 10 mm width are fitted for microbeam targeting. An additional motorised variable collimator is remotely operated, enabling rapid adaptation between large field (up to 40mm x 80mm) and small focal irradiations (3 mm x 3 mm).
In some cases, the target to be irradiated is located in an area where motion may cause significant displacement. To combat tumour motion, a rotating shutter that opens and closes in synchrony with movement coordinates X-ray delivery with respiration. This respiratory-gated dose is regulated by fibre-optic motion detection, and is used to deliver x-rays only during the resting part of the respiratory cycle. An integrated ion chamber ensures accurate real-time measurement of the dose during these gated treatments.
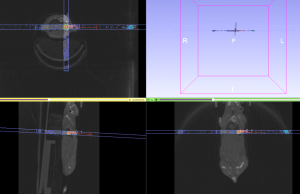
Muriplan image reconstruction software is used for CT image capture; and enables image rendering and segmentation, as well as coregistration with other imaging modalities, such as Bioluminescence or MR imaging, available in the adjacent Centre for Advanced Biomedical Imaging (CABI). Following 3D image reconstruction within Muriplan, anatomical structures can be precisely targeted, using arc or static beam delivery. The visualisation of dose distribution through different beam geometries enables radiation treatment to be planned in a clinically-relevant manner.
The SARRP includes a robotic specimen stage. Movement of the stage during irradiation facilitates targeted dose delivery and enables precise targeting through X-lateral, Y-longitudinal and Z-vertical axis and 360 degrees of rotation
Ongoing projects
Lung cancer is the second most common cancer in both males and females in the UK, with over 46,000 new cases diagnosed annually (CRUK). To improve treatment options for advanced stage patients, immunotherapies such as pembrolizumab are being used as a life-extending treatment in the case of metastatic disease.
Combining radiation with immunotherapy may enhance the host adaptive immune response, leading to reduction in tumour-immune evasion and increasing the curative potential of radiotherapy. With the objective of quantifying these enhanced therapeutic effects; immune-stimulatory outcomes following radiotherapy are being investigated. These include alterations to the immune compartment in the tumour microenvironment, effects on antigen presentation and T cell priming, and increased tumour-immune recognition. Experimental models are evaluated following radiotherapy via outcomes such as response to combined treatments, likelihood of tumour recurrence and changes to immune cell populations.
Collaborators: Professor Sergio Quezada (UCL), Dr Crispin Hiley (Crick/UCL), Dr Marquez Vasquez (UCL).
Whether patients receive radiotherapy varies according to the stage and the type of tumour at the time of treatment: Earlier stage tumours are more likely to be treated surgically, and later stages more likely to need radio- or chemo-therapy or combination treatments. However, as many as 50% of cancer patients are likely to receive radiotherapy at some point during treatment. New treatments will often be trialled against, or in addition to, radiotherapy, and preclinical testing that utilises targeted radiation increases the clinical relevance of the data obtained.
Preclinical testing frequently combines radiation with cancer-targeting agents that have been characterised in vitro to determine therapeutic potential and molecular mechanisms of action. Preclinical radiotherapy provides an essential validation step to progress the use of such compounds; allowing more rapid translation of compounds into clinical trials and providing confirmation of enhanced therapeutic effects. Combined with biomarker studies, this research promotes the identification of stratified patient populations for targeted therapies, maximising the potential benefits to patients during combined treatments.
Collaborators: Professor Sibylle Mittnacht (UCL), Dr Marcos Vasquez (UCL) and Dr Georgia Zoumpoulidou (UCL).
Dosimetry in preclinical irradiators is of key importance in evaluating radiation response in model systems. Historically, preclinical quality standards for measuring dose have lagged behind the more comprehensive methods utilised during clinical radiotherapy. Potentially, this may lead to variation between experiments conducted at different research sites. In addition, dose inconsistencies can adversely affect radiation response, and cause altered research outcomes.
Initiatives to improve measurement practices, including CRUK RadNet CoL RRU strategy for preclinical translational research, are aiming to increase awareness on the need for standardisation of dose measurement procedures, and improved reporting of dosimetric data of preclinical irradiations.
At UCL Cancer Institute, we introduced a quality program that includes periodical evaluation of beam quality (HVL) and monitoring of SARRP output. It also includes an appropriate dosimetry verification of the dose delivered by image-targeted irradiation plans, validated by participation in a traceable dosimetry audit. Dosimeters including an ion chamber/electrometer system (calibrated against the National Physical Laboratory primary standard for air kerma), alanine pellets and Gafchromic film, are currently used to facilitate these dosimetric evaluations.
Collaborators: Dr Anna Subiel (UCL), Professor Andy Nisbet (UCL) and Ileana Silvestre Patallo (UCL).





